EDITORIAL
ORIGINAL STUDIES
BACKGROUND. Vocal cord paresis in 59% of cases is a result of surgical interventions on the organs of the neck and chest. However, thyroid surgery is the main cause of them (up to 49% of cases). Unfortunately, the most tragic complication — bilateral recurrent laryngeal nerve injury in 80% is associated with thyroidectomy.
AIM. To determine the risk factors and causes of vocal cord paresis in patients after thyroid and parathyroid surgery. To analyze the clinical picture, catamnesis of postoperative vocal cord paresis.
MATERIALS AND METHODS. The study included patients who underwent thyroid and parathyroid surgery. Laryngeal mobility was assessed in all patients before and after surgery (transcutaneous ultrasound, videolaryngoscopy). Surgical interventions were performed by 8 endocrine surgeons with mandatory visualization of the recurrent laryngeal nerve. In the late postoperative period videolaryngoscopy was performed in patients with vocal cord paresis every month. Patients monitoring was discontinued upon recovery of laryngeal mobility.
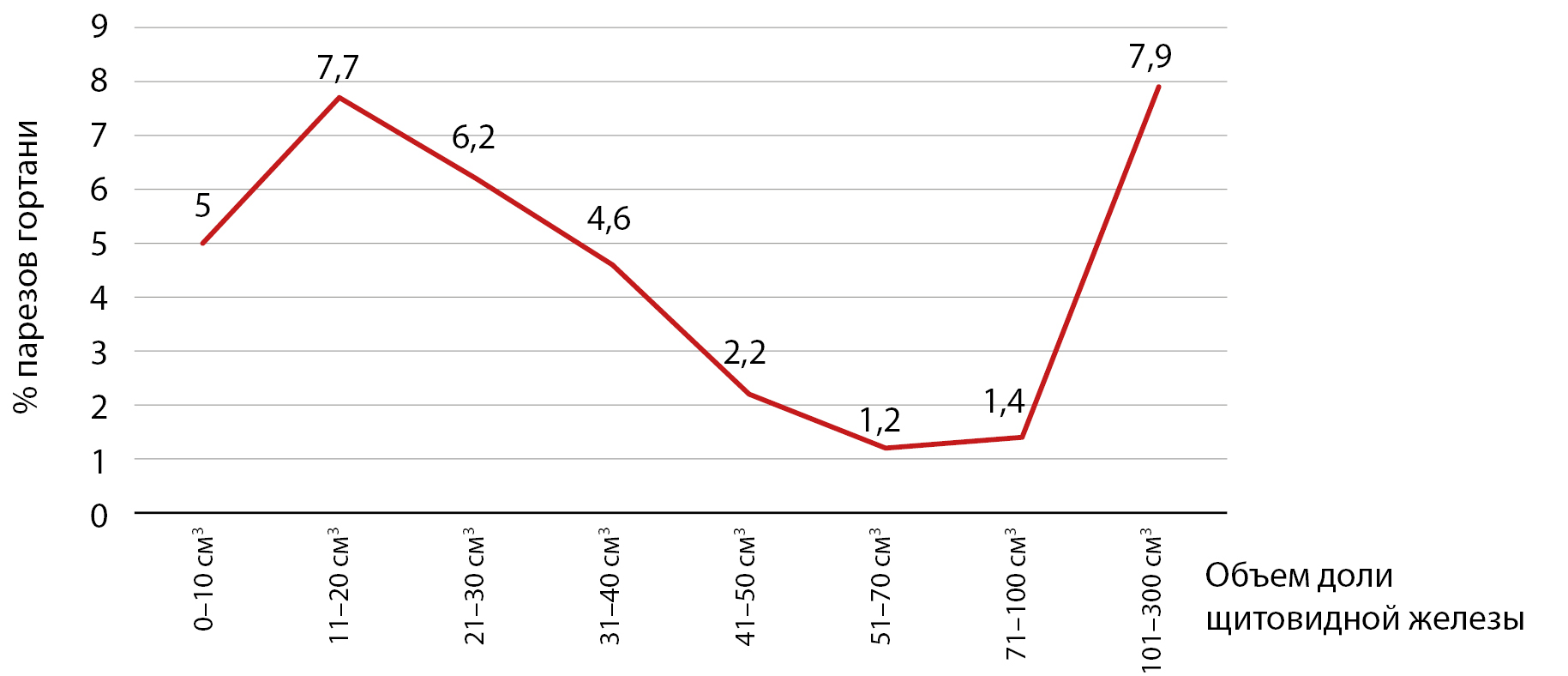
RESULTS. In the study identified 2682 (100%) recurrent laryngeal nerves and diagnosed 169 (6.3%) unilateral vocal cord paresis. Preoperative vocal cord paresis (type A) was found in 0.5% of patients. Postoperative vocal cord paresis due to carcinoma invasion (type B) were noted in 0.5% of cases. Type “C” included inadvertent postoperative vocal cord paresis, occurring in 5.3% of cases.
Factors such as sex, age, disease, chronic thyroiditis, increasing surgery, retrosternal location, and increased volume of the thyroid lobe did not elevate the level of postoperative vocal cord paresis (p>0.05). However, reoperation, progression of malignant processes and surgical technique influence the number of postoperative vocal cord paresis (p < 0.05).
Vocal cord paresis was characterized by the following clinical properties: negative Valsalva test — 68.1%, choke on liquid — 46.0%, breathlessness — 7.4%, and the voice did not change in 24.5% of patients. Recovery of laryngeal mobility was observed in 67.2% of patients. In 97.1% of cases complete recovery of motor function was noted within the first 3 months after surgery.
CONCLUSION. The clinical picture of vocal cord paresis in the early postoperative period ranging from asymptomatic forms to dysphagia and respiratory failure. Moreover, the symptoms and laryngoscopic findings are nonspecific (independent of the cause of recurrent laryngeal nerve injury), thus, not determining the prognosis for recovery of laryngeal mobility. However, in the long-term postoperative period indicators such as frequency of recovery, timing of recovery and volume of vocal cord mobility reflect three types of nerve damage — neurotmesis, neuropraxia, and axonotmesis.
RELEVANCE: thyroid surgery has always been particularly difficult. Today, surgeons are increasingly performing large-scale and complex hemi- and thyroidectomies. In cases of a malignant process, removal of the thyroid gland can be supplemented by central or lateral lymph dissection. Among the complications, damage to the recurrent laryngeal nerves occupies a special place due to its severity and potential to cause patient disability. The frequency of this complication, according to summary data, can reach up to 10%.
OBJECTIVE: to develop a safe method for visualizing recurrent and non-recurrent laryngeal nerves during various thyroid surgeries.
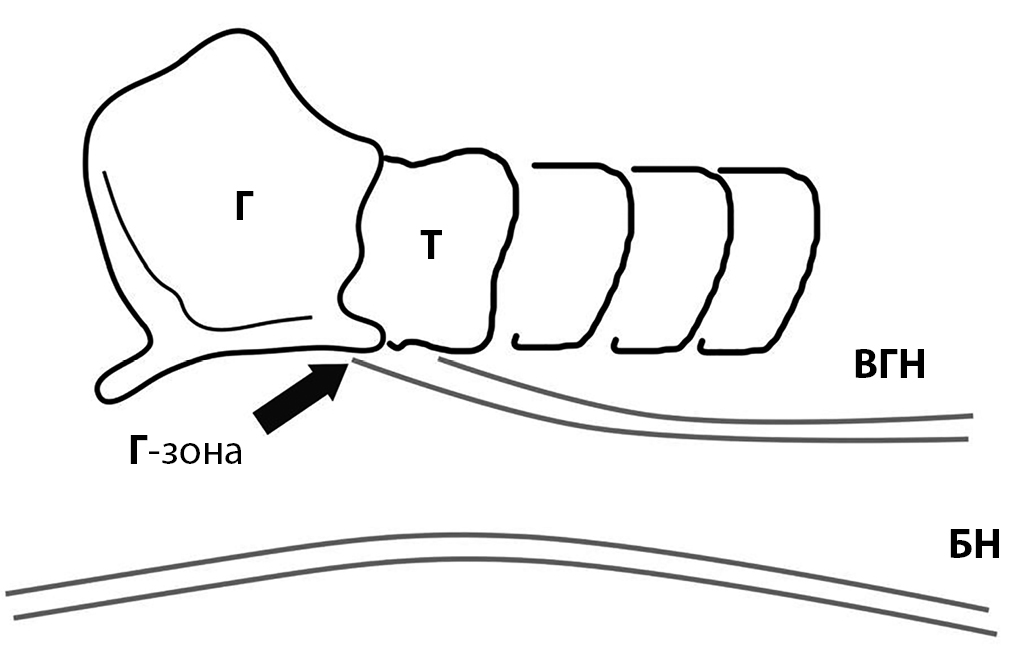
MATERIAL AND METHODS: the study analyzed treatment outcomes for 85 patients with various diseases of the thyroid gland treated at the Botkin hospital in 2024. Operations ranging from hemithyroidectomy to thyroidectomy with cervical lymphodissection were performed in the observed patients. During surgical treatment, microsurgical visualization of laryngeal nerves was performed using a method involving a virtual anatomical D-triangle to determine the search area in the paratracheal region. The D-triangle is defined as an isosceles obtuse triangle with its vertex at the laryngotracheal angle, formed by the lower border of the larynx, the lateral contour of the trachea (2 cm long), and the base connecting these lines.
RESULTS: analysis showed that the required surgical outcomes were achieved in all cases without the development of laryngeal paresis or paralysis. Key findings include recurrent laryngeal nerves with normal and anomalous locations being identified. An embryonic anomaly of the right recurrent laryngeal nerve was noted in 1 (1.2%) case. Fascial fixation of the recurrent laryngeal nerve by thyroid capsule bundles was found in 4 (4.7%) cases. Extraorgan branches of the right recurrent laryngeal nerve were observed in 3 (3.5%) cases. One (1.2%) case involved a small-diameter lesion of the nerve.
CONCLUSION: routine precision imaging of recurrent and non-recurrent laryngeal nerves using the proposed D-triangle method facilitates this challenging stage of thyroid surgery. The technique reduces the risk of laryngeal paresis and paralysis, ensuring safer outcomes for patients with various thyroid diseases.
BACKGROUND: When assessing the effectiveness of scar treatment, it is important to consider both the specialist’s assessment of the scar characteristics and the patient’s self-assessment of their condition. The Patient and Observer Scar Assessment Scale (POSAS) is a questionnaire recommended by international guidelines for evaluating the quality of scar formation, including after surgical treatment.
AIM: To perform linguistic and cultural adaptation of the Russian version of the POSAS 3.0 questionnaire and to test it in the Russian patient population with various thyroid pathologies.
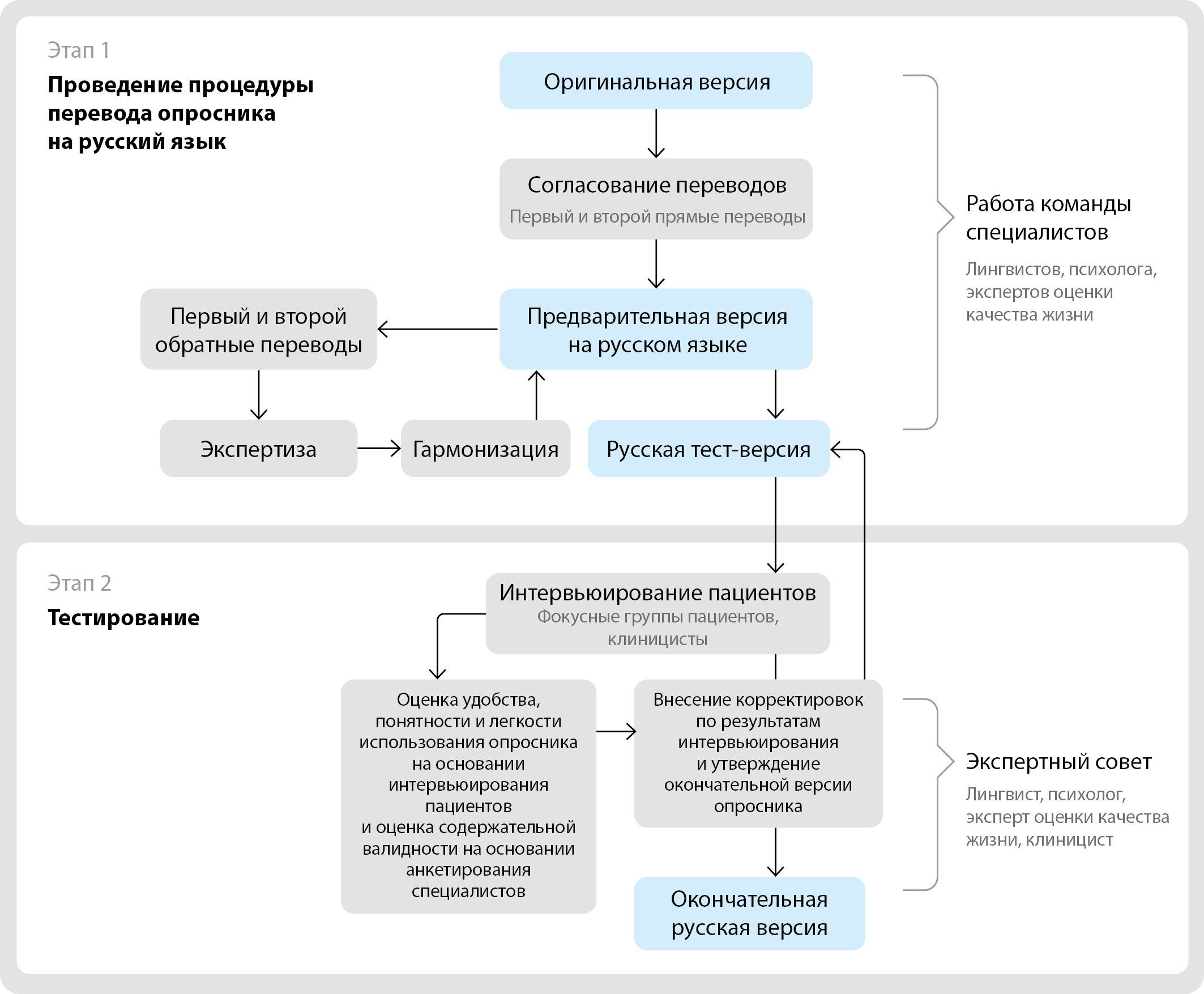
MATERIALS AND METHODS: The linguistic and cultural adaptation of the POSAS 3.0 questionnaire was performed in accordance with modern international recommendations. It included the procedure of forward and back translations, testing of the Russian versions via patients’ interviews, expert evaluation of Russian version by specialists and decentering.
RESULTS: The test version of the questionnaire was tested on 15 patients with various thyroid pathologies. Based on the interviews, an acceptable indicator of the external validity of the Russian version of the questionnaire was established. According to the survey of specialists (n = 9), its content validity was confirmed.
CONCLUSION: The linguistic and cultural adaptation process resulted in the final Russian version of the POSAS 3.0 questionnaire, which is equivalent to the original version and corresponds to the ethno-linguistic characteristics of the population. The use of the POSAS 3.0 questionnaire in research and clinical practice is possible after assessment of psychometric properties of these tools.
BACKGROUND: Hyponatremia is one of the most common and potentially dangerous complications following transnasal adenomectomy, making its timely detection and prevention critically important for improving treatment outcomes. Developing reliable models for predicting hyponatremia could reduce the risk of complications and enhance the quality of medical care for patients with pituitary adenomas.
AIM: To analyze preoperative and postoperative parameters of patients to develop a prognostic model for hyponatremia development after transnasal adenomectomy.
MATERIALS AND METHODS: A total of 122 patients were included in the analysis, of whom 38 (31%) were men. The patients were divided into two groups: those who developed hyponatremia by the 7th postoperative day and those who did not. The groups were comparable in terms of gender (p=0.425) and age (53 [34; 62] years vs. 44.5 [36; 56] years, p=0.172). A comparison of the groups was conducted across 42 parameters, including hormonal levels (ACTH, cortisol, TSH, free T4), the presence of cardiovascular diseases, carbohydrate metabolism disorders, and hypogonadism, the medication therapy administered, as well as tumor characteristics based on MRI data and surgical protocol details.
RESULTS: No differences were found between the groups for any parameter (p>0.001). The groups were subsequently compared by laboratory parameters relative to reference ranges (TSH/ACTH/cortisol/free T4 above, below, or within the reference interval), tumor characteristics (e.g., color, consistency, position relative to the pituitary gland), and tumor morphology. No significant differences were identified for any of the parameters analyzed (all p>0.001). Thus, the groups with and without hyponatremia on the 7th postoperative day did not differ statistically, making it impossible to construct a prognostic mathematical model for this complication.
CONCLUSION: The inability to predict postoperative hyponatremia based on preoperative parameters or surgical characteristics underscores the necessity of monitoring blood sodium levels until 10–14 days after transnasal adenomectomy.
BACKGROUND. Diabetic foot syndrome (DFS) significantly worsens the quality of life of patients, and is also a significant economic problem for healthcare. Understanding the clinical and laboratory characteristics of patients with DFS and type 1 diabetes mellitus (DM1) may be the key to prevention and timely detection of complications.
PURPOSE. To study the clinical and laboratory characteristics of patients with DFS suffering from DM1.
MATERIALS AND METHODS. A retrospective analysis of 759 case histories of patients with diabetes mellitus of the Limb Rescue Center at the V.P. Demikhov State Clinical Hospital in the period from 2019 to 2020 was carried out. The object of the study was a group of patients with DM1 (n=30). The statistical analysis was carried out using the STATISTICA 8.0 program.
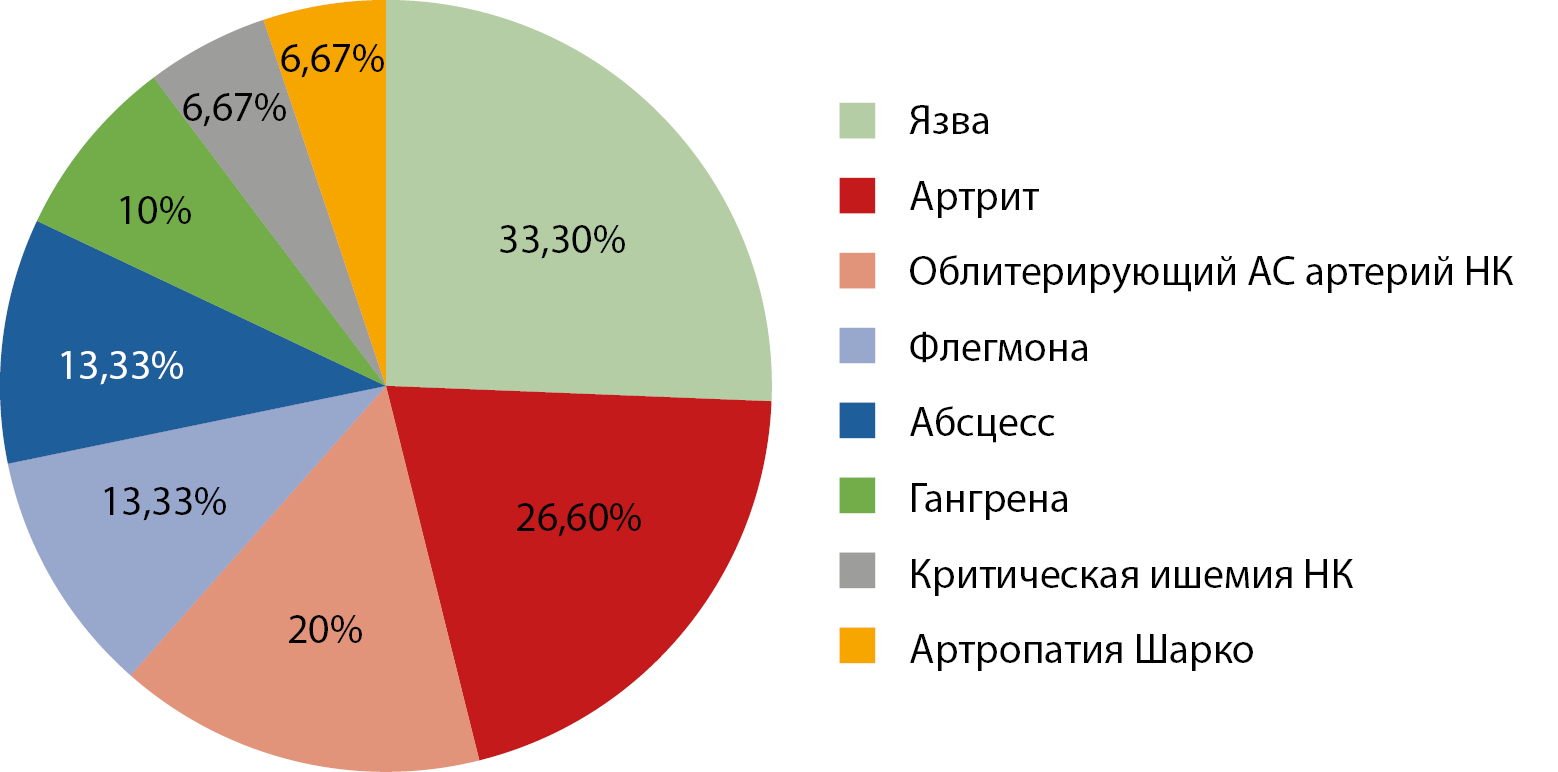
RESULTS. The average age of patients was 50.67±1.84 years (95% CI 46.89–54.44). 66.67% (n=20) of patients had a normal BMI, and the average BMI was 22.79±1.27 kg/m2 (95% CI 19.96–25.63). 86.7% had a long history of DM1. The median fasting plasma glucose was 13.1 mmol/l [7.1; 1.6]; and the average HbA1c was 8.71±0.26% (95% CI 8.18–9.25)). Almost half of the patients had microcytic anemia (47%, n=14). 66.67% (n=20) of patients already had a history of DFS. Hypertension was most common among the concomitant pathologies (50%, n=15) and atherosclerosis of the arteries of the lower extremities was almost as likely (46.67%, n=14). CHD (30%, n=9) and CKD (30%, n=9) were slightly less common among the studied patients as concomitant diseases. Only local treatment in the form of primary surgical treatment was provided mainly to patients with neuropatic form of DFS (46.67%, n=14). 10% (n=3) of patients underwent stenting, and 36.67% (n=11) underwent low amputation. The average duration of hospitalization was 11.55± 1.05 (95% CI 9.40–13.71) bed days.
CONCLUSION. Analysis of clinical and laboratory data showed that patients with DM 1 hospitalized at the limb rescue center had significant risk factors for the development of ulcerative necrotic pathology: decompensation of carbohydrate metabolism, dyslipidemia, arterial hypertension. Understanding the importance of correcting risk factors can prevent patients from developing pathology requiring surgical treatment, including amputation, which can help reduce the duration of hospitalization and, consequently, reduce the burden on healthcare in economic terms.

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License (CC BY-NC-ND 4.0).
ISSN 2310-3965 (Online)