Review
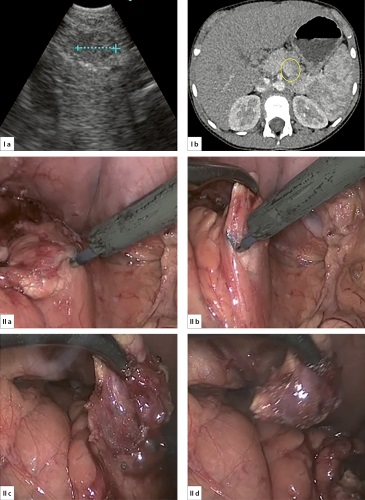
BACKROUND: Insulinoma is a tumor of β-cells of the islets of Langerhans, secreting an excessive amount of insulin, which is manifested by attacks of hypoglycemic symptoms Diagnosis of insulinomas localization in the pancreas can be extremely difficult and should include all available methods of radiation diagnosis. The only radical way to treat insulinoma is surgical. Traditionally, these operations were performed in the open version. There are only isolated publications on the performance of laparoscopic interventions in children with insulinomas.
AIM: To present our experience of using laparoscopic technologies in the treatment of children with insulinomas of various localizations.
MATERIALS AND METHODS: In the period from 2016 to 2023, 12 girls aged 7 to 17 years were operated on for pancreatic insulinoma. The average age of the patients was 12.5±3.1 years.
RESUITS: All operations were completed in the laparoscopic version, there were no conversions. There were no intraoperative complications. In the early postoperative period, 3 children had complications. Parapancreatic fluid accumulations in 2 cases were drained by transgastric endoscopic fine needle puncture. After enucleation of insulinoma from the hookshaped process of the pancreas, 1 child developed focal pancreatic necrosis, which required pylori-preserving pancreatoduodenal resection. In all other cases, the postoperative period proceeded smoothly. All children have achieved a good clinical effect in the form of relief of symptoms and the absence of episodes of hypoglycemia. There was no recurrence of the disease in the period from 1.5 to 5 years.
CONCLUSIONS: Experience shows that with the specified localization of insulinoma in the pancreas, laparoscopic operations can be performed using EUS and intraoperative sonography.
Original study
BACKGROUND: The combination of differentiated thyroid carcinoma (DTC) and Graves’ disease (GD) in childhood is extremely rare. According to the literature, the prevalence of DTC in adult GD is about 20%, and only a few cases have been described in children.
AIM: To determine the prevalence and describe the clinical morphologic features of thyroid carcinoma in children with GD.
MATERIALS AND METHODS: Retrospective study of 77 patients aged 10 to 17 years who underwent thyroidectomy for GD.
All patients underwent a comprehensive clinical-instrumental, cytologic and pathomorphologic study based on Endocrinology Research Centre in the period from January 2022 to September 2024.
RESULT: The incidence of DTC in children with GD was 10.4% (8 out of 77 patients), while in patients with nodules on the background of DTC – 21.7%. Interestingly, even in the absence of evidence of a thyroid nodule, the incidence of DTC was 5.5% and was detected only on pathomorphologic examination. According to the pathomorphologic stedy, the classical subtype of PTC was determined in 4 patients, papillary microcarcinoma – in 2 patients, follicular variant of PTC – in 1 patient, combination of follicular carcinoma and classical subtype of papillary carcinoma – in 1 child.
CONCLUSION: The high incidence of DTC in children with GD requires increased oncologic vigilance in their management. Fine-needle aspiration (FNA) of nodular masses belonging to EU-TIRADS categories 3-5 is a mandatory step in the examination. In the presence of nodular masses in the thyroid gland, surgical method of radical treatment of GD in children is preferable due to their high risk of malignancy.
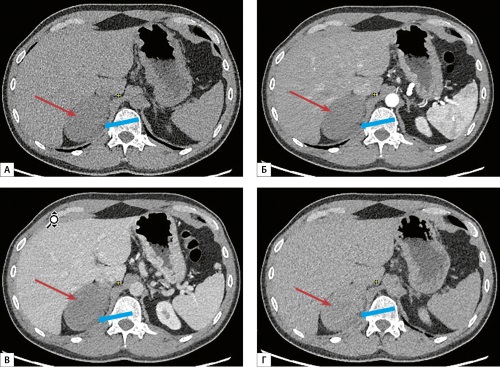
BACKGROUND: Currently, an annual study of venous glucose after night fasting is carried out to detect hypoglycemia for diagnosis the recurrence of insulinoma. However, hypoglycemia cannot always be achieved after night fasting if tumor is small. Previously continuous glucose monitoring (CGM) in diagnosis of recurrence of insulinoma was evaluated in small samples.
AIM: To evaluate the effectiveness of CGM in interstitium for the diagnosis of recurrent insulinoma (hypoglycemia) after surgery.
METHODS: Adult patients who underwent surgery for insulinoma and with remission in the early postoperative period were included. The glucose level in the interstitium was studied by CGM for a maximum of 14 days, and a single venous blood glucose test was performed after a night fasting. If hypoglycemia was detected by any method, a long-term fasting test to confirm the recurrence of hypoglycemic syndrome and imaging diagnostics to identify insulinoma were performed.
RESULT: The study included 29 patients after surgical treatment of insulinoma 3-69 months ago. Normoglycemia was determined in 28 patients after night fasting, while one had hypoglycemia, subsequently confirmed by a long-term fasting test. During the CGM, 25 patients had normoglycemia throughout the entire study period, while hypoglycemia was detected in 4 patients, and among them subsequent long-term fasting test confirmed it in three cases. During instrumental examination, pancreatic formation, different in location from the primary tumor, was detected in these three patients. Thus, the sensitivity of CGM relative to reference night fasting test is 100%, 95% CI (3%; 100%), specificity 89% (72%; 98%), positive predictive value 25% (1%; 81%), negative predictive value 100% (86%; 100%). During CGM no adverse events were detected.
CONCLUSIONS: CGM can be used effectively and safely to rule out hypoglycemia; and positive cases require subsequent long-term fasting test.
Clinical Case
A clinical case of neurofibromatosis 1 type in combination with pheochromocytoma in a 53-year-old woman with no family history of the disease is described. The diagnosis of neurofibromatosis 1 type was established on the basis of signs of the disease (glioma of the right optic nerve, epilepsy, hypertension, Lish nodules, osteoporosis). The diagnosis of pheochromocytoma was established according to the data of a multiple increase in the level of free metanephrines and normetanephrines in daily urine, a malignant CT phenotype of a tumor of the left adrenal gland, and confirmed by a pathomorphological examination. During genetic analysis, a variant HG38 not previously described in the literature in the heterozygous state was found in the NF1 gene in exon 38, leading to deletion of 4 nucleotides and a shift in the reading frame with a coverage depth of 170x. The variant is not found in the gnomAD population frequency database and most likely leads to loss of function of the corresponding copy of the gene, which makes it possible to attribute the pheochromocytoma in this case to the 2nd cluster of genetic abnormalities in paragangliomas. This case highlights the importance of timely diagnosis of neurofibromatosis type 1 to determine further follow-up and treatment plan. It also demonstrates the effectiveness of cooperation between specialists from different medical fields in the diagnosis and treatment of tumors secreting catecholamines, which can occur with neurofibromatosis 1 type.
As a rule, patients with a multi-nodular goiter are not regularly observed by doctors, the reason for seeking medical help is the presence of a growing formation on the neck or the development of compression syndrome. More often, such patients are referred for surgical treatment, namely for hemi- or total thyroidectomy. This study presents a clinical case of non-surgical treatment in stages using ethanol sclerase therapy and radiofrequency ablation (RFA), which allowed the organ to be preserved, while achieving the necessary cosmetic effect, there is no damage to surrounding tissues and organs. The combined treatment of diffuse nodular goiter made it possible to reduce the size of the neoplasm by 21 times from the initial one during the treatment period from 2019 to 2021, eliminated the cosmetic defect and compression syndrome. Sclerotherapy and RFA can act as an alternative to surgical methods, but without scarring of the neck. Interventional methods are effective in the treatment of thyroid nodules, including large ones.
Ganglioneuromas (GN) are rare benign neoplasms originating from neural crest tissue. These tumors are typically asymptomatic and are often detected incidentally during diagnostic imaging studies. Although the radiological characteristics of adrenal GNs are relatively well-studied, establishing an accurate diagnosis still remains a challenging task. Currently, the definitive diagnosis is established based on the morphological examination of postoperative material.
This publication presents a rare clinical case of an adrenal GN identified in a 35-year-old male. А mass in the right adrenal gland measuring 8.4×5.8×5.8 cm with a malignant CT phenotype and indirect signs of possible invasion was detected at an abdominal MSCT scan. Hormonal evaluation showed no evidence of excessive hormone secretion. Taking into account the set of characteristics of the tumor, which indicated a high risk of malignancy, the patient underwent surgical treatment, including thoracophrenolaparotomy and right adrenalectomy. Morphological examination revealed that the tumor consisted of interwoven bundles of mature Schwann cells with ganglion cell inclusions confirming the diagnosis of GN. The postoperative period was uneventful.
This clinical case highlights the difficulty in preoperative diagnosis of GN and underscores the need for comprehensive and thorough evaluation using all available diagnostic methods.

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License (CC BY-NC-ND 4.0).
ISSN 2310-3965 (Online)