ABSTRACT BOOK of ХХXIII Russian symposium on endocrine surgery with the participation of endocrinologists «Kalinin readings»
BACKGROUND: According to modern concepts [1], microRNAs modulate the expression of eukaryotic genes with different oncogenetic directions of action. according to the data from the scientifi literature [2–4], microRNA-146b, -199b can be used for typing thyroid neoplasms, -221, -223, -31, -375, -451a, -551b, etc. Nucleolar organizers (NOR) are sections of chromosomes that form a nucleolus inside the cell nucleus [5–7]. The condition of the regions of nucleolar ribosome organizers (AgNORs) is a marker of the rate of cell proliferation, since they are involved in the regulation of the mitotic cycle [8], and in thyroid pathology [9].
AIM: To evaluate the diagnostic significance of the level of expression of some microRNAs and the number of regions of nucleolar organizers in thyroid tissue in the case of follicular thyroid tumor of uncertain malignant potential (FT-UMP) to objectify approaches to the validity of the chosen surgical tactics.
MATERIALS AND METHODS: In our study of 3960 patients with surgery due to various thyroidopathies in 2018–2021 on the basis of the thyroid center of Chelyabinsk. 2063 patients were operated on for tumor pathology. In this group, in 98 cases (the study group), FT-UMP was diagnosed based on morphological criteria of neoplasm [10]. This accounted for 4.75% of all surgical tumor pathology during this time. The study group studied the profile, the level of microRNA expression by real-time PCR and the regions of nucleolar organizers in 98 cases of FT-UMP, which amounted to 4.75% of all those operated for thyroid tumors over four years.
RESULTS: In 29 (29.6%) cases, a microRNA spectrum characteristic of malignant neoplasms was registered in the tumor tissue. In the remaining 69 (70.4%) cases out of 98 observations, the spectrum and level of microRNA expression corresponded to follicular adenoma. Statistically significant differences in the average number of AgNORs and the ratio between the cell area and the number of AgNORs granules were revealed within the formed subgroups. The study found that an increase in the average number of AgNORs and the ratio of the core area to the number of silver nitrate granules in the 2nd subgroup relative to the 1st, as well as the presence of type II cells indicates the appearance of proliferating tumor cells in the neoplasm and can be considered as prognostic criteria for tumor malignancy. These results are consistent with the obtained indicators of molecular genetic research
CONCLUSION: The data can serve as additional criteria for assessing the proliferative activity of the follicular epithelium in thyroid neoplasia. Including clarifying the potential of malignancy. The conditionally malignant variant diagnosed before the operation will justify the need and scope of surgical intervention, and when identifying a set of criteria for conditionally benign HPV, it can be recommended to adhere to wait-and-see tactics.
BACKGROUND: Primary hyperparathyroidism (PHPT) is a common endocrinological disease that is characterized by autonomic increased synthesis of parathyroid hormone (PTH) with elevated or upper-normal levels of blood calcium [1]. In 80–85% of cases, the cause of sporadic PHPT is an adenoma of one parathyroid gland (PTG) (sigle-gland parathyroid disease), in 20–25% — a lesion of a larger number of PTGs (hyperplasia of all glands or double adenomas — multigland parathyroid disease) [2]. The complexity of clinical and laboratory prediction, low sensitivity of imaging methods, poor assessment of the radicalness of the operation by intraoperative monitoring of intact PTH (IMiPTH) are the components of the problem of multiple lesions in PHPT. Therefore, the improvement of existing and the development of new methods for diagnosing and treating this variant of the disease are urgent tasks of modern endocrine surgery.
AIM: To develop an algorithm for the diagnosis and treatment of PHPT, aimed at preoperative detection of multigland parathyroid disease.
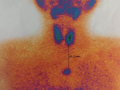
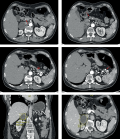
MATERIALS AND METHODS: The study was based on a study of a continuous sample of 208 patients, of which 34 with multigland parathyroid disease in PHPT, 95 with single-gland parathyroid disease in PHPT, 69 with secondary hyperparathyroidism on renal replacement therapy (RRT) with hemodialysis, and 10 with tertiary hyperparathyroidism on RRT of LT. The work was performed on the basis of clinical, laboratory, instrumental, morphological and immunohistochemical studies. The nature of the expression of the calcium-sensitive receptor and the vitamin D receptor in the studied groups was studied as a pathogenetic substantiation of the proposed algorithm [3]. Based on the study of clinical and laboratory parameters and the results of preoperative imaging methods, predictors of multigland parathyroid disease in PHPT [4,5] were established, and a method for differential diagnosis of PTG lesions in PHPT was developed [6]. In addition, the results of surgical treatment of patients with multiple PTG lesions in various clinical variants of hyperparathyroidism were studied [7]. RESULTS: The proposed algorithm is used when the diagnosis of PHPT is already established and there are indications for surgical treatment. First of all, the level of GFR (CKD-EPI) is assessed in conjunction with the results of the “gold standard” preoperative imaging methods (ultrasound and scintigraphy), with an assessment of the number of localized increased PTG and the consistency of the results of preoperative methods.
At a GFR level of more than 73 ml/min/1.73 m2, an increase of only 1 PTG according to the results of 2 imaging methods, provided that they are consistent, the PHPT variant is defined as a sigle-gland parathyroid disease. If there is an inconsistency between the 2 methods of preoperative imaging, we recommend calculating the scores according to the differential diagnosis scale for multiple lesions in PHPT [6]. At a GFR level of less than 73 ml/min/1.73 m2, an increase of >1 PTG according to the results of 2 imaging methods, we recommend calculating points according to the proposed scale [6].
With the established variant of PHPT — sigle-gland parathyroid disease, the patient undergoes selective parathyroidectomy (PTE) with IMiPTH. When iPTH drops to reference values, the test is considered positive, and the operation ends there. If the test result is negative, a second test is required after 10 minutes. In the event that the repeated test is also negative, then the patient is shown a bilateral neck exploration (BNE) in accordance with the tactics for multigland parathyroid disease (see below).
With the established variant of PHPT — multigland parathyroid disease, the following tactics are used:
- BNE with obligatory exploration of all four PTGs;
- Macroscopic assessment of the PTG found.
- When making a decision about 2 pathologically changed enlarged PTG, and 2 others are intact and not enlarged, a double PTE with IMiPTH is performed. If after the removal of 2 pathologically altered PTGs, the IMiPTH test is negative, then a second one is necessary after 10 minutes. In the event that the repeated test is negative, then from the 2 recognized intact ones, the least altered is determined and the scope of the operation is expanded to subtotal PTE (3.5 PTG), leaving ½ of the least altered PTG. The operation ends here.
- When deciding that 3 or more PTG are pathologically changed and enlarged, a subtotal PTE with IMiPTH is performed. In case of a negative IMiPTH test, the places of possible ectopic location of the PTG are examined: thyrothymic ligaments, upper thymus horns, fatty tissue along the carotid arteries. If there are no ectopically located PTGs in the indicated places, the operation is completed.
CONCLUSION: The proposed treatment and diagnostic algorithm is pathogenetically substantiated, aimed at preoperative detection of multiple PTG lesions in PHPT and will improve the quality of life of this group of patients by reducing the persistence of the disease.
BACKGROUND: Hyperparathyroidism (HPT) is a syndrome characterized by excessive synthesis of parathyroid hormone (PTH), an imbalance of phosphorus-calcium metabolism, and damage to target organs. Radical treatment of any clinical variant of HPT is surgical. In this regard, the assessment of the quality of life (QoL) of patients before and after surgery is an indicator that reflects the impact of the disease on the patient’s health and the effectiveness of the treatment.
AIM: To study QoL of patients with various clinical variants of HPT before and after surgical treatment.
MATERIALS AND METHODS: The single-center prospective study included patients operated on for primary (PHPT), secondary (SHPT) and tertiary HPT in 2019–2021. A comparison was made of preand postoperative QoL indicators with a sample comparable in sex and age from residents of the Irkutsk region.
RESULTS: The study included 100 patients, of which 13 had multiple lesions of the parathyroid glands (PTG) and 51 with solitary lesions in PHPT, 34 with SHPT and 2 with SHPT. Indicators QoL of patients with HPT before surgery is statistically significantly lower than in the region. The greatest decrease in QoL was found in the group of patients with multiple PTG lesions in PHPT. Improvement in QoL was achieved in 90% of the studied patients. Despite the identified complications, there was an improvement in QoL after surgery in case of achieving remission of the disease. Persistence of the disease is an outcome that does not allow for a statistically significant improvement in QoL after surgery for any type of HPT. Deterioration of QoL according to some indicators was found in 10% of patients. In patients with solitary PTG lesions in PHPT, deterioration in QoL is associated with postoperative hypocalcemia against the background of the «hungry bones» syndrome, and in patients with SHPT with a decrease in parathyroid hormone below population indicators.
CONCLUSION: The study demonstrates QoL of patients with various clinical variants of hyperparathyroidism before and after surgical treatment. The dynamics of QoL indicators depending on the nosology, volume, duration, outcome and complications of operations is shown.
Anthropometric data, indicators of laboratory and instrumental examinations were prospectively studied in 80 patients with primary hyperparathyroidism who were treated at the Republican Clinical Hospital for War Veterans of the Ministry of Health of Chuvashia. The quality of life of all patients with primary hyperparathyroidism was assessed before and after surgical treatment using two questionnaires: the SF-36 questionnaire and the standardized quality of life questionnaire for patients with PGPT — PHQol, an adapted Russian version of the quality of life questionnaire for primary hyperparathyroidism. As a result of the study, primary hyperparathyroidism was found to be a disease with a low level of detectability due to low awareness of practitioners, therefore, it often takes up to 10 years from the onset of the disease to diagnosis. It is necessary to introduce screening programs to determine the level of calcium in the blood. The disease primary hyperparathyroidism is of medical and economic importance, which pushes us to pay closer attention to this disease, to create a register of patients with primary hyperparathyroidism. Assessment of the quality of life before and after surgical treatment makes it possible to assess the subjective state of the patient, and also contributes to a patient-oriented approach in the management of patients with PGPT. The standardized questionnaire for assessing the quality of life in hyperparathyroidismPHQoL, its adapted and validated Russian version is a reliable method for studying the quality of life before and after surgical treatment of patients with PGPT, as well as for evaluating the effectiveness of surgical treatment.
Congenital adrenal dysfunction (CHD) is a variant of hereditary fermentopathies that lead to a violation of the synthesis of cortisol in the adrenal cortex. Late diagnosis of this pathology significantly impairs the quality of life of patients, and in some cases can lead to fatal consequences. The most common form of CHD, occurring in more than 90% of cases, is due to a deficiency of 21-hydroxylase, which is responsible for the synthesis of deoxycorticosterone and 11-deoxycortisol. The prevalence of this form is 1:10,000 to 1:20,000 newborns in the world, in Russia — 1:9500. In second place is the deficiency of 11β-hydroxylase (hypertonic form of HCHD), which affects the synthesis of cortisol. This form of the disease occurs in about 1:100,000 newborns in the world, and in Russia the prevalence of this form is unknown [1].
The cause of any form of CHD is mutations in the genes responsible for the synthesis of enzymes or transport proteins involved in the synthesis of cortisol. 11β-hydroxylase is synthesized in the zona fasciculata of the adrenal cortex and is regulated by adrenocorticotropic hormone by a negative feedback mechanism. 11β-hydroxylase deficiency (hypertonic form of HCHD) develops as a result of mutations in the CYP11B gene located on chromosome 8. This mutation blocks the enzymatic conversion of 11-deoxycortisol to cortisol, as well as deoxycorticosterone (DOC) to corticosterone, leading to the accumulation of DOC, which has mineralocorticoid activity. It is the excess of deoxycorticosterone that causes an increase.
In 21-hydroxylase deficiency, the clinical picture is primary adrenal insufficiency (deficiency of glucoand mineralocorticoids). The clinical picture of mineralocorticoid deficiency includes salt loss syndrome: arterial hypotension, tachycardia, adynamia, fibrillary muscle twitching, dryness and decreased skin turgor, cyanosis and marbling of the skin. Glucocorticoid deficiency is manifested by muscle weakness, fatigue, hyperpigmentation of the skin. With a deficiency of 11β-hydroxylase, due to an increase in the level of deoxycorticosterone, there is no deficiency of mineralocorticoid activity, on the contrary, against the background of clinical signs of glucocorticoid insufficiency, an increase in blood pressure may be observed. Hyperandrogenism is characteristic of both forms of CHD. Symptoms of hyperandrogenism in females: virilization of the external genitalia, amenorrhea, severe alopecia and hirsutism. In undiagnosed cases of CHD, patients with a female karyotype have a male phenotype.
Original study
Fine needle aspiration (FNA) biopsy has been a powerful tool in the preoperative diagnosis of thyroid nodules for more than 60 years. The Bethesda scale standardizes the results of cytology and is a tool for interaction between the laboratory and the clinician. At the same time, there is a stratification of ultrasound signs of thyroid lesions according to the TI-RADS scale. In this regard, it became necessary to determine the diagnostic value of ultrasound signs of thyroid lesions, stratified by TI-RADS, in comparison with the results of a biopsy, classified by the Bethesda scale.
AIM: a comparative assessment of the results of FNA and ultrasound in determining indications for the surgical treatment of thyroid nodules.
MATERIALS AND METHODS: for 2018–2021 in the surgical department of the SCC №2 of the Petrovsky National Research Centre of Surgery, 859 FNA were performed. For comparative analysis, 141 patients who underwent surgery for thyroid nodules were selected. All patients at the preoperative stage underwent FNA with stratification of the results according to the Bethesda scale and ultrasound of the thyroid gland with stratification according to the EU-TI-RADS scale.
RESULTS: FNA showed high diagnostic accuracy and sensitivity, preoperative thyroid ultrasound had high specificity, but low sensitivity. The high diagnostic value of FNA was confirmed by statistical analysis of the obtained data (OR 31.29 95% CI 2.20–4.69, RR 13.28 95% CI 1.46–3.71). When analyzing preoperative ultrasound, it was not possible to obtain reliable statistical results (OR 2.99 95% CI 0.34-1.85, RR 1.97 95% CI 0.23-1.12).
CONCLUSION: Ultrasound of the thyroid gland cannot replace FNA in thyroid nodules. Biopsy remains the main diagnostic method for nodular goiter. The main objective of TI-RADS-stratified ultrasound is to select patients for subsequent FNA.
BACKGROUND: It was impossible to predict the development of hypocalcemia following parathyroidectomy (PTE) in patients with primary hyperparathyroidism (PHPT) until now. Hypocalcemia may be accompanied by myalgia, generalized seizures up to tetany, and arrhythmias. Hypocalcemia following PTE can be prevented by preoperative cholecalciferol supplementation. However, patients with severe hypercalcemia above 3 mmol/L do not receive vitamin D due to the risk of hypercalcemia progression. Despite the existing data showing the safety of cholecalciferol therapy in case of mild elevation of serum calcium, not all patients are prescribed vitamin D supplementation, probably due to the lack of a suitable tool to assess the postoperative hypocalcemia risks.
AIM: To design a mathematical model and a software tool for predicting hypocalcemia 1–3 days post-PTE in PHPT patients using the patient’s demographic and clinical data, laboratory test results and preoperative therapy status.
MATERIALS AND METHODS: This retrospective study included 478 PHPT patients diagnosed with adenomas and carcinomas of the parathyroid gland (PTG) who underwent radical PTE between 1993–2010 or 2018–2020 at the Endocrinology Research Centre. The following parameters were analyzed: sex; age; laboratory markers prior to calcimimetic and antiresorptive therapy: PTH, total calcium, phosphorus; osteocalcin (OC), alkaline phosphatase (ALP), C-terminal telopeptide of type 1 collagen. Also we analyzed 25-hydroxyvitamin D (25(OH)D); bone mineral density (BMD) measured by X-ray densitometry; medical history of low-energy fractures; preoperative therapy with denosumab, bisphosphonates, cinacalcet, cholecalciferol. Categorical gradient boosting (CatBoost) was built to predict the risk of postoperative hypocalcemia.
RESULTS: The prevalence of severe osteoporosis is higher in the postoperative hypocalcemia group compared to the nonhypocalcemia group (27% vs. 15%), wherein the frequency of preoperative administration of cholecalciferol in this group is lower (8% vs. 25%). A CatBoost model was built to predict postoperative hypocalcemia using 13 predictors (sex, age, PTH, serum total calcium, phosphorus, OC, BMD reduction, 25(OH)D, administration of cholecalciferol, bisphosphonates, denosumab, and cinacalcet. The proposed model http://194.87.111.169/hypocalcemia for post-PTE hypocalcemia in PHPT patients achieved the following metrics: positive predictive value 73.3%-86.7%; negative predictive value 74.9%-89.3%.
CONCLUSION: The model can be used to choose the appropriate preand postoperative approaches for patients who undergo rPTE.
Clinical Case
Multiple endocrine neoplasia type 1 (MEN-1) is the orphan disease caused by the metachronous tumors of endocrine and non–endocrine organs. The first most frequent feature of the syndrome is primary hyperparathyroidism, however, manifestation from other components is also possible. Different medical specialists should know about this pathology because its clinical course is often varied.
This clinical case of non-classical manifestation of MEN-1 demonstrates the difficulties of diagnostics, comprehensive examination and treatment of the main components of the syndrome. Timely laboratory, instrumental and genetic diagnostics plays an important role in the prevention of complications, improving the quality of life and prognosis of patients.

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License (CC BY-NC-ND 4.0).
ISSN 2310-3965 (Online)